Our Hand Surgical Unit has treated two young women for serious injuries to the ulnar nerve sustained during removal of contraceptive implants. To avoid permanent injuries, it is important that such implants are inserted correctly, and that patients are referred to a hand surgeon if it is suspected that an implant may prove difficult to remove.
One form of contraception available in Norway is the Nexplanon® implant – a 2 mm × 4 cm soft plastic rod recommended for subcutaneous placement in the medial upper arm (1). We present the case histories of two women with slender upper arms who sustained serious left-sided ulnar nerve injuries during the removal of such implants.
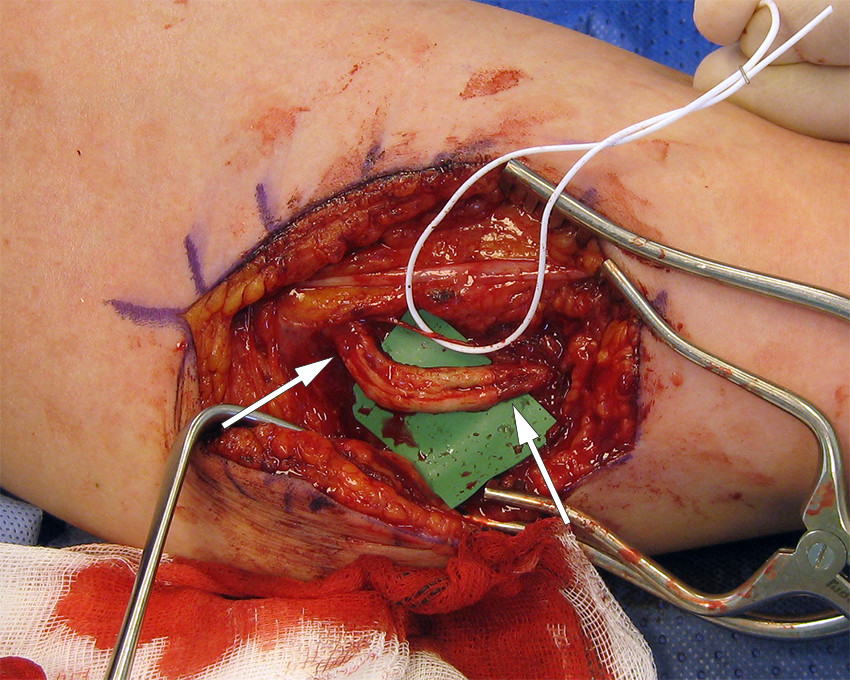
Patient 1 was referred to a hand surgeon with ulnar nerve dysfunction following removal of a contraceptive implant. According to the referral, the implant had been non-palpable and had therefore been removed under general anaesthesia with the aid of an X-ray image intensifier. The patient reported waking up with severe pain in her upper arm radiating to the ulnar aspect of the hand. Neurophysiological testing had been requested and performed prior to the referral. The results, together with those of the clinical examination, suggested a complete lesion of the ulnar nerve at the midhumerus level. There was a 2 cm long scar overlying the sulcus between the biceps and triceps, where local percussion triggered intense, radiating pain. At surgery 2.5 months after removal of the implant, we discovered a neuroma-in-continuity. A neuroma is a nodule consisting of disorganised scar tissue and nerve fibres. It can take the form of an end-neuroma (upon complete transection of the nerve) or a lesion-in-continuity, where a nodule of scar tissue is usually found in continuity with an apparently intact nerve. In the present case, only a single ulnar fascicle remained intact. The neuroma was resected, and the 2.5 cm defect was reconstructed using a nerve graft (sural nerve) harvested from the left leg (Figure 1). Two years later, the patient still had pronounced pain and limited sensory and motor function in the hand, and had fallen out of work.
Patient 2 had had a contraceptive implant removed under local anaesthesia, and immediately experienced painful paraesthesias, loss of sensibility and reduced strength in the two ulnar fingers. Clinical and neurophysiological examination after one week revealed findings consistent with a subtotal lesion of the ulnar nerve, and she was referred for surgery. Exploration 1.5 months after removal of the implant revealed the ulnar nerve to be entrapped in scar tissue including a superficial cutaneous nerve and the basilic vein. The structures were carefully separated, revealing no clear loss of continuity. Three years after surgery, the patient's grip strength and sensibility were still reduced, but she had little pain.
Discussion
The use of contraceptive implants is increasing in Norway, with over 19 000 such implants inserted in 2016 (2). The procedure can be performed under local anaesthesia by a variety of healthcare professionals. The implants provide effective contraception for a period of three years (1). Nerve injuries are rare (3), but can be very serious, as our case histories illustrate. A systematic review identified 10 articles describing 14 nerve injuries in 12 patients (4). Twelve injuries occurred during removal of the implant and two upon implantation. The most common scenario was for a nerve to be pulled after having been mistaken for the implant. Most injuries involved the medial antebrachial cutaneous or median nerves, followed by the ulnar nerve. The basilic vein and brachial artery can also be affected. Median, and especially ulnar nerve injuries at this level in adults have a poor prognosis (5, 6).
Surprisingly few recommend placement in areas other than the medial upper arm, but the inner thigh and anterior abdominal wall have been suggested (7, 8). When inserting an implant in the upper arm, it is essential to follow the protocol carefully to ensure that the implant is inserted subdermally and, in particular, that it is positioned sufficiently posterior to the sulcus between the biceps and triceps muscles. A distance of 3–5 cm is recommended, but could well be increased further to ensure that the implant is overlying the triceps muscle. A study of 40 cadaveric arms provides support for this practice (9).
Upon removal, the implant must be stabilised by palpation. The distal part of the implant is pushed upwards so that the skin forms a 'tent' over the end. A small incision can then be made close to the rod, enabling it to be removed without difficulty. If the implant is non-palpable, it may have been inserted too deeply or it may have migrated within the upper arm or intravascularly (10, 11). Contraceptive implants that are difficult to palpate can be localised with X-rays (they contain barium sulphate) or ultrasound. Deeper positioning increases the risk of nerve damage. In the event of a non-palpable implant, the patient should be referred to a surgeon with expertise in peripheral nerve surgery (12) so that the implant can be removed in the safest way possible. In Norway, surgery on peripheral nerves is performed by hand surgeons. Surgical access must be increased to 4–5 cm to allow the contraceptive implant to be visualised and to provide a sufficient view of the surrounding structures prior to removal.
In summary, it is important that healthcare professionals who insert contraceptive implants follow the guidelines carefully, and that they receive sufficient training in the procedure. For the removal of an implant that is difficult to palpate, the patient should be referred to a surgeon experienced in operating close to nerves and blood vessels. If nerve damage is suspected, the closest Hand Surgical department should be contacted by telephone, and the patient referred for urgent care. Further investigation (such as neurophysiological testing) is unnecessary and leads to delay in treatment. The waiting time for surgery is an important prognostic factor, particularly in partial nerve injuries where the development of a neuroma can quickly complicate reconstruction.
The patients have consented to the publication of this article.
Thank you to expert photographer Øystein Horgmo, University of Oslo, for preparing the image.
- 1.
Felleskatalogen. Nexplanon 68 mg implantat til subkutan bruk. https://www.felleskatalogen.no/medisin/nexplanon-msd-560036 Accessed 12.2.2021.
- 2.
Folkehelseinstituttet. Dobling i bruk av p-stav blant unge kvinner. https://www.fhi.no/nyheter/2017/dobling-i-bruk-av-p-stav-blant-unge-kvinner/ Accessed 12.2.2021.
- 3.
Darney P, Patel A, Rosen K et al. Safety and efficacy of a single-rod etonogestrel implant (Implanon): results from 11 international clinical trials. Fertil Steril 2009; 91: 1646–53. [PubMed][CrossRef]
- 4.
Laumonerie P, Blasco L, Tibbo ME et al. Peripheral nerve injury associated with a subdermal contraceptive implant: Illustrative cases and systematic review of literature. World Neurosurg 2018; 111: 317–25. [PubMed][CrossRef]
- 5.
Post R, de Boer KS, Malessy MJA. Outcome following nerve repair of high isolated clean sharp injuries of the ulnar nerve. PLoS One 2012; 7: e47928. [PubMed][CrossRef]
- 6.
Ruijs AC, Jaquet JB, Kalmijn S et al. Median and ulnar nerve injuries: a meta-analysis of predictors of motor and sensory recovery after modern microsurgical nerve repair. Plast Reconstr Surg 2005; 116: 484–94. [PubMed][CrossRef]
- 7.
Osman N, Dinh A, Dubert T et al. A new cause for iatrogenic lesion of the ulnar nerve at the arm: contraceptive hormonal implant. Report of two cases. Chir Main 2005; 24: 181–3. [PubMed][CrossRef]
- 8.
Wechselberger G, Wolfram D, Pülzl P et al. Nerve injury caused by removal of an implantable hormonal contraceptive. Am J Obstet Gynecol 2006; 195: 323–6. [PubMed][CrossRef]
- 9.
Iwanaga J, Fox MC, Rekers H et al. Neurovascular anatomy of the adult female medial arm in relationship to potential sites for insertion of the etonogestrel contraceptive implant. Contraception 2019; 100: 26–30. [PubMed][CrossRef]
- 10.
Diego D, Tappy E, Carugno J. Axillary migration of Nexplanon®: Case report. Contraception 2017; 95: 218–20. [PubMed][CrossRef]
- 11.
Rowlands S, Mansour D, Walling M. Intravascular migration of contraceptive implants: two more cases. Contraception 2017; 95: 211–4. [PubMed][CrossRef]
- 12.
Odom EB, Eisenberg DL, Fox IK. Difficult removal of subdermal contraceptive implants: a multidisciplinary approach involving a peripheral nerve expert. Contraception 2017; 96: 89–95. [PubMed][CrossRef]
Jeg har alltid undret meg over at man anbefaler plassering over de viktigste nerve-kar-banene til overekstremiteten. Kanskje en annen plassering burde anbefales?
Hei, vi undres også over dette. I artikkelen har vi gjengitt den anbefalte plasseringen. Plassering medialt på overarmen er kanskje gunstig fra et kosmetisk perspektiv, men komplikasjonene, når de oppstår, blir desto mer alvorlig med denne plasseringen. Få har anbefalt andre plasseringer, men låret eller bukveggen er nevnt som alternative muligheter.