Main findings
We found a number of powerful narratives of adverse life experiences among 70 patients examined at a regional Norwegian centre for morbid obesity.
A recurring feature in many of the categories of experiences was a constant 'state of alarm' for long periods of the person's life, starting from childhood.
Obesity is one of the great health challenges of our time. This development is linked to complex dynamics between dietary habits, physical activity, physiology, genetics and epigenetics in a globalised world, where the access to high-energy foods has become virtually unlimited for many people (1, 2). Moreover, solid international evidence indicates that stressful life events can contribute significantly to the development of obesity through emotional as well as physiological processes (3–9). In 1998, the American ACE study (Adverse Childhood Experiences) showed a dose-response relationship between traumatic childhood experiences and morbid obesity in adulthood (5). In recent years, a number of meta-analyses have confirmed and expanded on the correlations between traumatic childhood experiences and obesity in adulthood (8, 9). In the material from the Nord-Trøndelag Health Study (HUNT, 2006–08) we found a similar dose-response relationship between the self-reported degree of childhood difficulties and a number of forms of morbidity, including obesity, later in life. In the HUNT study, 4.1 % per of the adult participants reported to have had a 'difficult' or 'very difficult' childhood (6).
Patients with morbid obesity (BMI ≥ 40 kg/m2 or BMI ≥ 35 kg/m2 with weight-related comorbidity) can be referred by their GP to the specialist health service, where they will be offered guidance on lifestyle and possibly also bariatric surgery (10). In recent years, a number of meta-analyses have confirmed and expanded on the correlations between traumatic experiences in childhood and obesity in adulthood (8, 9). However, this knowledge has not been incorporated in Norwegian clinical practices to any great extent, and is only mentioned as vague recommendations in the guidelines for health personnel (10).
At the Regional Centre for Morbid Obesity in Bodø, interviews about stressful life experiences have for some years been included in the examination. This practice is based on knowledge about and clinical experience of how such an approach can help provide better insight into the complex causes of obesity (11). Many of the patients have given accounts of major life stresses, and a number of them have been referred to trauma therapy. This is the background for our project, which also includes a thesis in the medical study programme at the Norwegian University of Science and Technology (12).
The objective of this project was to document and analyse the information that patients who were undergoing assessment at a centre for morbid obesity in Norway chose to provide to an experienced doctor who signalled openness to discussing difficult life experiences.
Material and method
The data stem from discharge summaries of patients recently assessed for morbid obesity at the Regional Centre for Morbid Obesity in Bodø. The examination is described in Box 1. In the summer of 2018, an invitation to participate in the study was sent to the 200 patients who were the last to have been examined at the centre. The attending doctor and a research nurse retrieved de-identified data from the discharge summaries of those patients who had consented to participate. The study was approved by the Regional Committee of Medical and Health Research Ethics (REK Nord 2018/1002) and the Norwegian Centre for Research Data (NSD).
Tertiary health service
Patients are normally referred by the local hospital, assessed according to the following criteria:
-
BMI ≥ 40 kg/m2 or ≥ 35 kg/m2 with comorbidity
-
The patient wishes conservative or surgical treatment
-
Treatment attempts have been made locally for six months
Assessment
The assessment normally lasts for one to three days
The entire clinical examination is undertaken by the same senior consultant and comprises:
-
General medical history, including questions about stressful life experiences
-
Clinical examination, including dental health status
-
Relevant laboratory tests
Adverse life experiences
As part of the patient's medical history, the doctor addresses the following issues (open questions):
-
Feeling of security in the home as a child and adolescent
-
Social participation with peers
-
Physical activity in childhood and adolescence
-
School performance
-
Life events in the period prior to a dramatic weight gain, if relevant
The notes describing life events are normally taken during the consultation in collaboration between the doctor and the patient, and vary from a few lines to half a page per patient.
No standardised interview guide or questionnaire is used to map the patient's life experiences, and no questions focus directly on trauma.
Seventy patients (57 women) returned a signed consent form and were included in the study. Background information on the included patients is shown in Table 1. We considered the sample to be relevant, varied and well suited for the purposes of the study (13).
Table 1
Characteristics of the 70 participating patients who were under examination for morbid obesity at the Regional Centre for Morbid Obesity in Bodø. Number if not otherwise specified.
| Variable | Value | |
|---|---|---|
| Sex | ||
| Women | 57 | |
| Men | 13 | |
| Age categories | ||
| 20–39 years | 15 | |
| 40–59 years | 45 | |
| 60–79 years | 10 | |
| Marital status | ||
| Married/co-habiting | 47 | |
| Education | ||
| Completed primary/lower secondary education | 23 | |
| Completed upper secondary education | 33 | |
| Completed higher education | 13 | |
| Unknown | 1 | |
| Employment | ||
| Gainfully employed | 33 | |
| Receiving disability benefit, in full or in part | 20 | |
| Other | 17 | |
| BMI (kg/m2), average (range) | 43 (30–63) | |
| Maximum weight (kg), average (range) | 133 (103–201) | |
Analyses
The method is inspired by interpretative phenomenological analysis (14, 15). All co-authors reviewed the material independently and identified preliminary categories of stressful life experiences. The material was subsequently reviewed by all authors jointly, whereby diverging interpretations were discussed and the final categories formulated. Categories that coincided directly with existing research in this area were identified first (5). We then defined some new categories in light of the existing literature. The attending doctor participated in the final phase of the analysis and validated the final categorisation. The stressful life events are reported as keywords and with no reference to sex and age to ensure anonymisation.
Results
The analysis produced twelve categories of stressful life events (Box 2).
1. Substantial feeling of insecurity (39 %)
2. Feeling of emotional neglect by parent (41 %)
3. Witness to violence (9 %)
4. Exposure to physical violence (26 %)
5. Exposure to psychological violence (34 %)
6. Exposure to sexual abuse/assault (29 %)
7. Exposure to bullying (29 %)
8. Serious relationship rupture (66 %)
9. Substance abuse by caregiver or partner (24 %)
10. Stressful care responsibilities (27 %)
11. Traumatic encounter with a dentist/health service (24 %)
12. Other personally significant trauma (21 %)
Figure 1 shows the distribution of stressful/adverse life experiences (number of categories) among the 70 participants. The categories are described in Box 2. Examples of the twelve experience categories are given in Table 2.
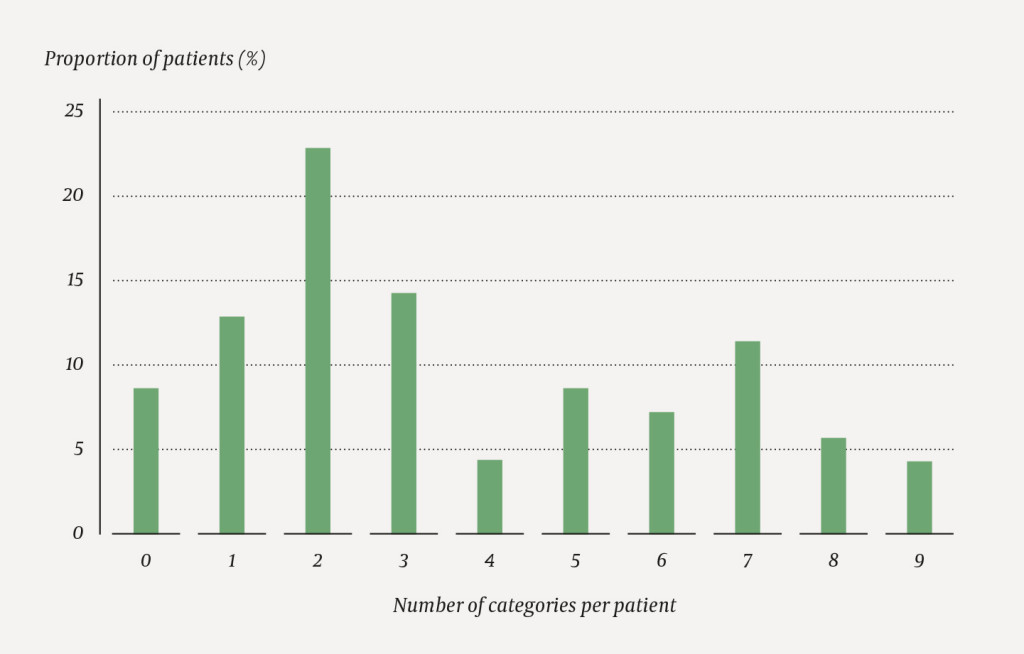
Table 2
Examples of individual, documented experiences in each of the twelve categories, represented by different patients in the study. To ensure anonymity, these are given as keywords and without any reference to age or sex.
| Category | Category content | Example (keywords) |
|---|---|---|
| 1. Substantial feeling of insecurity | Explicit description of feelings of fundamental insecurity early in life, with various underlying causes. | Insecurity in the home during adolescence, partly traumatising. |
| 2. Feeling of emotional neglect | Explicit description of perceived lack of care by one or both parents in childhood and adolescence. | As a child having been told by their mother that they were unwanted and should never have been born. |
| 3. Witness to violence | Having witnessed violence between parents in childhood. | As a child having feared being beaten by their father. Having witnessed their father being violent to their mother. |
| 4. Exposure to physical violence | Physical violence in childhood and adulthood. Mainly girls having been exposed to violence from their father or women exposed to violence by their partner. | Exposure to extreme violence by their father during childhood/adolescence. Involvement of child welfare services. |
| 5. Exposure to psychological violence | Threats, harassment and control by an intimate partner. | Was controlled and ruled over, later threatened with murder by their partner. |
| 6. Exposure to sexual abuse/assault | Rape in childhood or adulthood and/or experience of incest. | Persistent exposure to severe sexual abuse by their father and other adults. |
| 7. Exposure to bullying | Bullying by peers in school, including physical violence. Some have also been exposed to bullying by parents or teachers. | Severe bullying during long periods in school, with physical violence nearly every day. Nobody intervened. |
| 8. Serious relationship rupture | Loss of or separation from persons in significant, close relationships. Approximately half of the stories involve dramatic deaths or the death of someone close. More than half involve stressful relationship ruptures – involving either the patient's parents or the patients themselves in adult age. | Loss of a close relative in a dramatic accident during childhood. |
| 9. Substance abuse by caregiver or partner | Significantly affected by living with a caregiver/partner prone to substance abuse. | Periodically left alone with an alcoholic parent with large mood swings. |
| 10. Stressful care responsibilities | Care of children with special needs, sole carer for multiple children while in a poor financial situation and/or difficult relationship, care responsibility for spouse, early care responsibility for parents/siblings in adolescence. | Sole breadwinner. Financial problems, Very little sleep over many years. |
| 11. Traumatic encounter with a dentist/health service | Painful procedures, physical coercion during a visit to a dentist/doctor, a dentist who appeared to be intoxicated. | Odontophobia after a tooth extraction without anaesthetic as a child. |
| 12. Other personally significant trauma | Stories that do not fit into any of the other categories, but that the patients have described as highly stressful. | Notification of a serious disease with a possibly short life expectancy. |
Of our 70 participants, 64 (91 %) reported at least one significantly stressful life experience, and 39 (56 %) three or more types of various kinds. The most frequent were serious relationship ruptures, lack of care by parents and significant insecurity in childhood (Box 2). Serious relationship ruptures concerned loss of or separation from important persons close to the patient. This included deaths under dramatic circumstances, as well as stressful relationship ruptures involving the patient's parents or the patients themselves. Mental illness, substance abuse or violence were often part of the picture. Altogether 36 patients (51 %) reported to have been exposed to one or more types of violence or sexual abuse (categories 3–6), and 17 reported substance abuse in a close relationship (category 9). In connection with a check of their dental status, 33 (47 %) respondents reported to have odontophobia, of whom 17 (24 %) reported distressing experiences with a dentist during childhood or adolescence (category 11).
Discussion
In a sample of 70 patients in a Norwegian regional centre for morbid obesity, we divided the adverse and stressful life experiences reported by these patients into twelve categories. More than one-half of the patients had experiences that fitted into three or more of these categories. The most frequent were serious relationship ruptures, significant insecurity in childhood and a feeling of lack of care by parents. These were followed by a series of more specifically defined experiences, such as sexual abuse or having witnessed violence. As illustrated by Figure 1 and Table 1, the data material includes a number of complex life stories that describe series of stressful and interwoven experiences, summarised in keywords. The experience of relationship ruptures, violence and insecurity in early life not infrequently recurs in new constellations in the patients' adult life.
The study design was chosen because we wanted to explore a topic that international research highlights as important, but of which there is little knowledge in a Norwegian context (16). The participant group was heterogenous in terms of age, marital status, education and employment status, which indicates that the findings may have transfer value to similar patient groups. The proportion of women (81 %) was somewhat higher than the proportion in the Regional Centre for Morbid Obesity in Bodø where the study was conducted (70 %). It is difficult to ascertain whether the participants were significantly different in other respects from those who did not respond to the invitation.
The objective of the study was not to obtain generally valid prevalence data or draw any direct conclusions with regard to causal links between trauma and obesity. However, the study provides insight into what a sample of 70 patients with morbid obesity chose to reveal to an experienced doctor who provided space for a dialogue on adverse life experiences. The results should be seen in light of the fact that underreporting of trauma and abuse appears to be common, in clinical practice as well as in research (16, 17). The participants themselves considered these experiences as relevant in the clinical situation in question, and they contributed actively to their documentation.
During the analysis we were aware of our preconceptions and sought to the best of our ability to avoid prejudiced interpretations. We recognised that important nuances in the individual narratives could easily be lost or misinterpreted. Many narratives indicated complex experiences that could be subsumed under more than one category. The experiences were as far as possible categorised in direct consistency with the discharge summary. For example, information on the loss of a parent (category 8) was not categorised also as a feeling of insecurity in childhood (category 1), unless this had been explicitly described.
The analysis aimed to identify different categories of stressful life experiences that were clinically relevant. Such an analytical process can be driven by existing theory and evidence, and contribute to the development of new theories (14). The analysis was influenced by the group of authors' general knowledge of and research on correlations between life experiences and illness (6), (18–19).
Many of the categories (numbered 2, 4–9 and 12 in Box 2) could immediately be related to three key international studies (5, 20, 21). Moreover, the material provided the basis for defining some further categories (numbered 1, 3, 10 and 11), which could also be related to relevant documentation (see examples below). International literature in this area includes clinical research, basic research and epidemiological studies (12, 16). A number of publications document general associations between adverse experiences on the one hand and emotionally driven eating patterns and development of obesity on the other (4). There is a rapidly growing insight into the physiology that links stress to metabolic syndrome, appetite regulation and obesity (22). Furthermore, some epidemiological studies show associations between obesity and one or more trauma categories (referred to in 12).
A persistent mental 'state of alarm' seems to be a common denominator for many of the categories of experiences. Categories 1 and 2 point towards a fundamental lack of existential security early in life. The biological 'costs' of such a state of alarm feature prominently in modern stress research, including the allostatic load model. It describes the links between long-term stress, physiological dysregulation and development of disease, including obesity (23, 24). A feeling of insecurity and uncertainty is a key feature also in Hemmingson's obesity model (4). The ACE study showed a dose-response relationship between traumatic life experiences and morbid obesity (5). Later studies have confirmed these associations for sexual abuse, other forms of violence, emotional maltreatment or neglect, and substance abuse in the home (3, 7, 9). Relationship ruptures in the form of early loss of a parent increase the risk of development of obesity, irrespective of other stressful life events (25, 26). Bullying and obesity are mutually related (27, 28). Persistent, stressful care responsibilities are associated with physiological load, and an association with obesity is therefore plausible (29).
Our material includes several examples of poor dental health and odontophobia. Childhood adversity is associated with chronic systemic inflammation, which may interact with a poor diet and poor dental hygiene (30). Experience of violence and abuse predispose for odontophobia (31). Stressful childhood experiences may thus increase the risk of poor dental and oral health by way of a number of different mechanisms (30, 31).
An important finding in this study is that many participants reported multiple types of stressful life experiences and thus illustrated the relevance of the term 'complex traumas', not least with regard to the conditions of vulnerable children's upbringing (32). Another prominent finding was that participants who had experienced violence or abuse in childhood were also exposed to new incidents in adult life – so-called re-victimisation (33).
We hope that the study can motivate clinicians to be open and attentive in their encounters with severely obese patients. Addressing negative life experiences and trauma in relevant clinical settings does not lead to re-traumatisation (16, 17). A trauma-sensitive medical history that does not immediately seek to elicit certain types of information can provide space for consequential information without appearing as intrusive (34), and can help provide deeper and more adequate insight into the complexity that underlies an obesity problem. Such insight can reinforce the patient's self-insight and self-esteem and reduce the stigma and shame associated with obesity. This is health-promoting in itself (11, 35, 36). Current standardised patient pathways do little to facilitate broad, trauma-sensitive assessment and treatment of morbid obesity and the complex health problems associated with this diagnosis. Achieving a professional consensus about suitable new working methods is a considerable challenge. An integrated approach requires not only a well-functioning logistical collaboration across the current boundaries between somatic and mental health services; it also requires an updated and non-dualistic understanding of body and disease (19).
The authors wish to thank Lotte Hvas at the Research Unit for General Practice, University of Copenhagen, and Geir W. Jacobsen, professor emeritus at the Norwegian University of Science and Technology, for their valuable advice during the preparation of the manuscript.
Kai Brynjar Hagen's work on this project was supported by a stipend from the General Practice Research Committee.
The article has been peer reviewed.
- 1.
Brandkvist M, Bjørngaard JH, Ødegård RA et al. Quantifying the impact of genes on body mass index during the obesity epidemic: longitudinal findings from the HUNT Study. BMJ 2019; 366: l4067. [PubMed][CrossRef]
- 2.
WHO. Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight/ Accessed 11.5.2020.
- 3.
Følling IS, Solbjør M, Helvik AS. Previous experiences and emotional baggage as barriers to lifestyle change - a qualitative study of Norwegian Healthy Life Centre participants. BMC Fam Pract 2015; 16: 73. [PubMed][CrossRef]
- 4.
Hemmingsson E. A new model of the role of psychological and emotional distress in promoting obesity: conceptual review with implications for treatment and prevention. Obes Rev 2014; 15: 769–79. [PubMed][CrossRef]
- 5.
Felitti VJ, Anda RF, Nordenberg D et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med 1998; 14: 245–58. [PubMed][CrossRef]
- 6.
Tomasdottir MO, Sigurdsson JA, Petursson H et al. Self-reported childhood difficulties, adult multimorbidity and allostatic load. A cross-sectional analysis of the Norwegian HUNT Study. PLoS One 2015; 10: e0130591. [PubMed][CrossRef]
- 7.
Stensland SØ, Thoresen S, Wentzel-Larsen T et al. Interpersonal violence and overweight in adolescents: the HUNT Study. Scand J Public Health 2015; 43: 18–26. [PubMed][CrossRef]
- 8.
Danese A, Tan M. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatry 2014; 19: 544–54. [PubMed][CrossRef]
- 9.
Hemmingsson E, Johansson K, Reynisdottir S. Effects of childhood abuse on adult obesity: a systematic review and meta-analysis. Obes Rev 2014; 15: 882–93. [PubMed][CrossRef]
- 10.
Nasjonale faglige retningslinjer: Forebygging, utredning og behandling av overvekt og fedme hos voksne. Rapport IS-1735. Oslo: Helsedirektoratet, 2010. https://www.helsedirektoratet.no/retningslinjer/overvekt-og-fedme-hos-voksne/Overvekt%20og%20fedme%20hos%20voksne%20–%20Nasjonal%20faglig%20retningslinje%20for%20forebygging,%20utredning%20og%20behandling.pdf/_/attachment/inline/24ec824b-646d-4248-951f-db6b867ce6cb:4e0740b933ffd5bc03c8f0fdcab00b4135fe4ae9/Overvekt%20og%20fedme%20hos%20voksne%20–%20Nasjonal %20faglig%20retningslinje%20for%20forebygging,%20utredning%20og%20behandling.pdf Accessed 11.5.2020.
- 11.
Hagen KB. Lessons on causality from clinical encounters with severely obese patients. I: Anjum RL, Copeland S, Rocca E, red. Rethinking Causality, Complexity and Evidence for the Unique Patient. A CauseHealth Resource for Health Care Professionals and the Clinical Encounter. Dordrecht: Springer Nature, 2020.
- 12.
Gundersen IF, Stranden E. Livshistorier og fedmeutvikling. Hovedoppgave, medisinstudiet NTNU, Trondheim 2019. https://hdl.handle.net/11250/2679715 Data accessed 10.11.2020.
- 13.
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: Guided by Information Power. Qual Health Res 2016; 26: 1753–60. [PubMed][CrossRef]
- 14.
Kvale S. The qualitative research interview: A phenomenological and and a hermeneutical mode of understanding. J Phenomenological Psychol 1983; 14: 171–96. [CrossRef]
- 15.
Smith JA, Jarman M, Osborn M. Doing interpretative phenomenological analysis. I: Murray M, Chamberlain K, red. Qualitative Health Psychology: Theories and Methods. Kap. 14. London: SAGE Publications Ltd, 1999.
- 16.
Mason SM, Bryn Austin S, Bakalar JL et al. Child maltreatment's heavy toll: The need for trauma-informed obesity prevention. Am J Prev Med 2016; 50: 646–9. [PubMed][CrossRef]
- 17.
Becker-Blease KA, Freyd JJ. Research participants telling the truth about their lives: the ethics of asking and not asking about abuse. Am Psychol 2006; 61: 218–26. [PubMed][CrossRef]
- 18.
Kirkengen AL, Næss AB. Hvordan krenkede barn blir syke voksne. 3. utg. Oslo: Universitetsforlaget, 2015.
- 19.
Getz L, Kirkengen AL, Ulvestad E. Kroppsliggjøring av erfaring og mening- belastende erfaringers innvirkning på menneskets biologi. I: Mæland JG, red. Sykdommers sosiale røtter. Oslo: Gyldendal Akademisk, 2020: 205–30.
- 20.
Mäkinen T, Laaksonen M, Lahelma E et al. Associations of childhood circumstances with physical and mental functioning in adulthood. Soc Sci Med 2006; 62: 1831–9. [PubMed][CrossRef]
- 21.
Surtees PG, Wainwright NWJ. The shackles of misfortune: social adversity assessment and representation in a chronic-disease epidemiological setting. Soc Sci Med 2007; 64: 95–111. [PubMed][CrossRef]
- 22.
Michels N. Biological underpinnings from psychosocial stress towards appetite and obesity during youth: research implications towards metagenomics, epigenomics and metabolomics. Nutr Res Rev 2019; 32: 282–93. [PubMed][CrossRef]
- 23.
McEwen BS. Brain on stress: how the social environment gets under the skin. Proc Natl Acad Sci U S A 2012; 109 (Suppl 2): 17180–5. [PubMed][CrossRef]
- 24.
Cedillo YE, Murillo AL, Fernández JR. The association between allostatic load and anthropometric measurements among a multiethnic cohort of children. Pediatr Obes 2019; 14: e12501. [PubMed][CrossRef]
- 25.
Lynch BA, Agunwamba A, Wilson PM et al. Adverse family experiences and obesity in children and adolescents in the United States. Prev Med 2016; 90: 148–54. [PubMed][CrossRef]
- 26.
Alciati A, Caldirola D, Grassi M et al. Mediation effect of recent loss events on weight gain in obese people who experienced childhood parental death or separation. J Health Psychol 2017; 22: 101–10. [PubMed][CrossRef]
- 27.
Baldwin JR, Arseneault L, Odgers C et al. Childhood bullying victimization and overweight in young adulthood: A cohort study. Psychosom Med 2016; 78: 1094–103. [PubMed][CrossRef]
- 28.
Puhl RM, Latner JD, O'Brien K et al. Cross-national perspectives about weight-based bullying in youth: nature, extent and remedies. Pediatr Obes 2016; 11: 241–50. [PubMed][CrossRef]
- 29.
Epel ES, Blackburn EH, Lin J et al. Accelerated telomere shortening in response to life stress. Proc Natl Acad Sci U S A 2004; 101: 17312–5. [PubMed][CrossRef]
- 30.
Boyce WT, Den Besten PK, Stamperdahl J et al. Social inequalities in childhood dental caries: the convergent roles of stress, bacteria and disadvantage. Soc Sci Med 2010; 71: 1644–52. [PubMed][CrossRef]
- 31.
Willumsen T. The impact of childhood sexual abuse on dental fear. Community Dent Oral Epidemiol 2004; 32: 73–9. [PubMed][CrossRef]
- 32.
Braarud HC, Nordanger DØ. Komplekse traumatisering hos barn: en utviklingspsykologisk forståelse. Tidsskr Nor psykologforen 2011; 48: 968–72.
- 33.
Frugaard Stroem I, Aakvaag HF, Wentzel-Larsen T. Characteristics of different types of childhood violence and the risk of revictimization. Violence Against Women 2019; 25: 1696–716. [PubMed][CrossRef]
- 34.
Raja S, Hasnain M, Hoersch M et al. Trauma informed care in medicine: current knowledge and future research directions. Fam Community Health 2015; 38: 216–26. [PubMed][CrossRef]
- 35.
Daly M, Sutin AR, Robinson E. Perceived weight discrimination mediates the prospective association between obesity and physiological dysregulation: Evidence from a population-based cohort. Psychol Sci 2019; 30: 1030–9. [PubMed][CrossRef]
- 36.
Vadiveloo M, Mattei J. Perceived weight discrimination and 10-year risk of allostatic load among US adults. Ann Behav Med 2017; 51: 94–104. [PubMed][CrossRef]