In cost-benefit analyses, hip arthroplasty is ranked as one of the most successful medical and surgical treatments available (1, 2). Hip arthroplasty has been shown to give arthrosis patients a considerable reduction of pain as well as improved functional capability, at a lower cost than other forms of treatment (3). Nevertheless, the frequency of primary total hip arthroplasties varies significantly in different countries (4). These can be difficult to compare, however, since they often date from different periods of time and have been estimated without taking demographic differences into account. Previous reports have indicated that the number of hip arthroplasties caused by rheumatic disorders is declining (5) – (8), which may be due to improved drugs. On the whole, however, there is a clearly increasing frequency of hip arthroplasty in the Western countries. This has been documented for all the Nordic countries (9), Australia (10), Canada (11, 12) and the US (13). Within some countries, considerable regional differences in age-standardized rates have been documented (12, 14) – (17). In Norway, the prevalence of primary hip arthroplasty within different regions is unknown. Hence, the purpose of this study was to investigate whether the prevalence of primary total hip arthroplasty varied according to place of residence. We therefore compared the frequency of hip arthroplasties in the population according to place of residence, distributed among the regional health enterprises and county of residence in the years 1989 – 2008. We also wished to focus on changes in the prevalence over time.
Material and methods
In September 1987, the Norwegian Arthroplasty Register (18) started to record information on primary and revision hip arthroplasties (19, 20). This information is submitted to the register on paper (not electronically) by orthopaedic surgeons in all hospitals in Norway that perform this type of surgery. Compared to the number of operations reported to the Norwegian Patient Register, a total of 97 per cent of all primary hip arthroplasties were reported to the register in the period 1999 – 2002 (21). Prior to 1989, the registration procedure did not comprise all hospitals. In this study we therefore included primary hip arthroplasties performed in the period from January 1989 to December 2008, with the exception of operations performed on patients with no known place of residence (n = 37). The study was based on information on hip arthroplasties reported to the arthroplasty register. Information on the patients’ last known address as of 31 December 2008 was collected from the National Population Register, and demographic data were supplied by Statistics Norway (22).
Analyses
The annual unadjusted rate of primary total hip arthroplasties for the years 1989 – 2008 and for the periods 1989 – 90, 1991 – 95, 1996 – 2000, 2001 – 05 and 2006 – 08 was estimated as the number of operations divided by the population mean (average of the population at the beginning and at the end of the year) in Norway. Subdivisions have to the largest extent possible been undertaken in five-year intervals in order to allow for a comparison with other studies. The annual age and gender standardized rate was estimated by way of direct standardization (23), using the gender and age distribution (0 – 39, 40 – 49, 50 – 59, 60 – 69, 70 – 79, 80+ years) in Norway as the standard population. The annual rate for each period of time was also estimated for various diagnoses that may lead to arthroplasty, for each of the regional health enterprises and counties, as well as for sub-groups defined by gender and age for the primary operation. Even though different countries may have widely differing age distributions, the choice of a common standard population may still provide comparable figures for prevalence. An annual age-standardized rate was therefore also established on the basis on an estimated European standard population (24). Rate ratio (RR) values for the changes in prevalence over time and between geographical areas were estimated using Poisson regression, with the period 1991 – 95 as reference. These analyses were adjusted for gender and age, which were grouped as described above. P values less than 0.05 were assumed to be statistically significant. Analyses were undertaken with the aid of the software package SPSS 16.0 (SPSS Inc., Chicago, IL).
Results
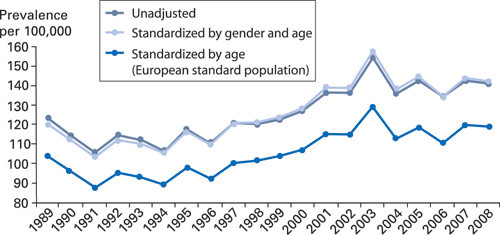
During the period of study, a total of 112,514 hip arthroplasties were performed in Norway. We observed an increase over time in the annual age and gender standardized frequencies of primary total hip arthroplasties (fig 1), from 109 operations per 100,000 inhabitants in 1991 – 95 to 140 in 2006 – 08 (RR = 1.28; 95 % confidence interval 1.25 – 1.30) (e-tab 1). This increase was at its strongest during the second half of the 1990s, and since then, only minor changes have been observed (fig. 1). The highest frequency was observed in 2003, with 157 operations for each 100,000 of the population. The differences between the standardized and the unadjusted rate remained minor during the entire period of study (fig 1).
E
-table 1 Gender and age standardized frequency 1 for primary total hip arthroplasties per 100,000 inhabitants, by period of time
| No. of prostheses |
1989 – 1990 |
1991 – 1995 |
1996 – 2000 |
2001 – 2005 |
2006 – 2008 |
RR ² (95 % CI) 2006 – 08 vs. 1991 – 95 |
||
| Total |
112,514 |
116 |
109 |
121 |
143 |
140 |
1.28 (1.25 – 1.30) |
|
| Gender |
||||||||
| Men |
34,479 |
79 |
76 |
80 |
96 |
99 |
1.30 (1.26 –1.35) |
|
| Women |
78,035 |
146 |
137 |
154 |
181 |
173 |
1.27 (1.24 –1.30) |
|
| Age |
||||||||
| 0 –39 |
2,056 |
4.3 |
4.1 |
4.2 |
4.2 |
4.4 |
1.08 (0.94 – 1.24) |
|
| 40 – 49 |
4,438 |
36 |
33 |
32 |
38 |
42 |
1.27 (1.16 – 1.39) |
|
| 50 – 59 |
13,783 |
142 |
117 |
124 |
151 |
155 |
1.33 (1.25 – 1.40) |
|
| 60 – 69 |
31,456 |
391 |
366 |
401 |
433 |
435 |
1,18 (1.14 – 1.23) |
|
| 70 – 79 |
43,921 |
602 |
576 |
632 |
786 |
758 |
1.32 (1.28 – 1.36) |
|
| 80+ |
16,860 |
312 |
332 |
400 |
500 |
458 |
1.37 (1.31 – 1.44) |
|
| Diagnosis ³ |
||||||||
| Idiopathic coxarthrosis |
81,510 |
77 |
74 |
85 |
109 |
109 |
1.46 (1.43 – 1.50) |
|
| Rheumatoid arthritis |
3,390 |
4.0 |
4.2 |
4.0 |
3.7 |
3,1 |
0.74 (0.66 – 0.83) |
|
| Sequelae femoral neck fracture |
11,690 |
16 |
14 |
14 |
12 |
10 |
0.70 (0.66 – 0.75) |
|
| Sequelae congenital dysplasia |
8,203 |
10 |
8.9 |
8.4 |
9.6 |
9,5 |
1.05 (0.98 – 1.13) |
|
| Sequelae congenital dysplasia with dislocation |
815 |
2.3 |
1.4 |
0.7 |
0.4 |
0,4 |
0.31 (0.23 – 0.41) |
|
| Sequelae Perthes’ disease/ epiphysiolysis |
1,480 |
1.6 |
1.6 |
1.6 |
1.8 |
1,8 |
1.12 (0.95 – 1.31) |
|
| Ankylosing spondylitis |
476 |
0.5 |
0.5 |
0.6 |
0.5 |
0,5 |
0.82 (0.61 – 1.11) |
|
| Fracture |
1,103 |
0.3 |
0.3 |
0.7 |
3.0 |
3,0 |
9.60 (7.44 – 12.0) |
|
| Osteonecrosis of the femoral head |
1,597 |
0.6 |
0.9 |
1.5 |
3.6 |
3,6 |
3.99 (3.37 – 4.17) |
|
| Other |
2,572 |
2.3 |
2.4 |
2.7 |
3.1 |
3,1 |
1.16 (1.02 – 1.31) |
|
| [i] | ||||||||
[i] ¹ Gender and age distribution in Norway 1989 – 2008 as standard (when relevant)
² Rate ratio (RR) adjusted for gender and age (when relevant). Poisson regression
³ More than one cause may have been reported to the Norwegian Arthroplasty Register
The age-adjusted frequency of hip arthroplasties was lower for men than for women, totalling 99 per 100,000 men and 173 for each 100,000 women. The frequency of hip arthroplasties increased over time for all age groups over 40 years, but was least marked in the age group 60 – 69 years. The increase in frequency was stronger for hip prosthetics implanted because of idiopathic coxarthrosis (RR = 1.46) than what was observed for the total material (e-tab 1).
County of residence and regional health enterprises
An increase in frequency was evident in all the regional health enterprises and counties (tab 2). In our comparison of prevalence in 1991 – 95 and 2006 – 08, we found the greatest increase among inhabitants of the Helse Nord health region (RR = 1.49; 95 % CI: 1.40 – 1.59). On the other hand, Helse Nord has had the lowest frequency throughout the entire period of study (fig 2). At the county level, we found the smallest increases among inhabitants of Rogaland (RR = 1.13; 1.05 – 1.21) and Telemark counties (RR = 1.13; 1.03 – 1.24), and the largest increase in Nordland county (RR = 1.86; 1.70 – 2.04) (tab 2).
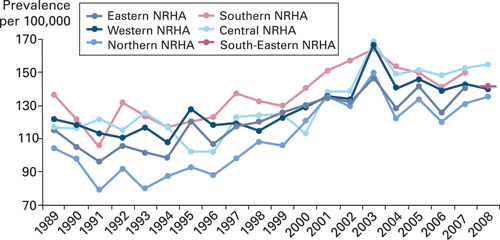
Table 2
Gender and age standardized frequency 1 for primary total hip arthroplasties per 100,000 inhabitants, by place of residence and period of time
| Regional health enterpriseCounty |
No. of prostheses |
1989 – 1990 |
1991 – 1995 |
1996 – 2000 |
2001 – 2005 |
2006 – 2008 |
RR² (95 % CI) 2006 – 08 vs. 1991 – 95 |
| Helse Øst³ |
39,125 |
111 |
104 |
120 |
137 |
134 |
1.28 (1.24 – 1.32) |
| Østfold |
6,433 |
113 |
111 |
111 |
131 |
136 |
1.23 (1.13 – 1.32) |
| Akershus |
10,220 |
107 |
105 |
127 |
140 |
133 |
1.24 (1.17 – 1.32) |
| Oslo |
10,463 |
81 |
88 |
107 |
120 |
120 |
1.34 (1.26 – 1.43) |
| Hedmark |
6,355 |
144 |
120 |
138 |
158 |
162 |
1.36 (1.25 – 1.47) |
| Oppland |
5,654 |
154 |
117 |
130 |
152 |
135 |
1.16 (1.06 – 1.27) |
| Helse Sør³ |
24,678 |
129 |
120 |
132 |
155 |
147 |
1.23 (1.18 – 1.28) |
| Buskerud |
6,612 |
132 |
115 |
127 |
155 |
148 |
1.26 (1.17 – 1.37) |
| Vestfold |
5,770 |
114 |
11 |
132 |
142 |
145 |
1.30 (1.20 – 1.42) |
| Telemark |
5,153 |
128 |
127 |
133 |
164 |
144 |
1.13 (1.03 – 1.24) |
| Aust-Agder |
2,992 |
132 |
133 |
140 |
164 |
172 |
1.29 (1.15 – 1.44) |
| Vest-Agder |
4,151 |
146 |
119 |
136 |
158 |
140 |
1.18 (1.07 – 1.31) |
| Helse Vest |
21,795 |
120 |
115 |
121 |
144 |
141 |
1.22 (1.17 – 1.28) |
| Rogaland |
8,175 |
126 |
118 |
122 |
144 |
135 |
1.13 (1.05 – 1.21) |
| Hordaland |
10,444 |
108 |
110 |
119 |
142 |
140 |
1.27 (1.20 – 1.35) |
| Sogn og Fjordane |
3,176 |
148 |
127 |
127 |
156 |
164 |
1.31 (1.17 – 1.46) |
| Helse Midt-Norge |
16,824 |
117 |
116 |
118 |
149 |
152 |
1.31 (1.25 – 1.37) |
| Møre og Romsdal |
6,315 |
115 |
111 |
110 |
147 |
143 |
1.29 (1.19 – 1.39) |
| Sør-Trøndelag |
6,561 |
116 |
109 |
116 |
141 |
154 |
1.40 (1.30 – 1.51) |
| Nord-Trøndelag |
3,948 |
122 |
139 |
135 |
169 |
165 |
1.19 (1.08 – 1.31) |
| Helse Nord |
10,092 |
101 |
86 |
104 |
134 |
129 |
1.49 (1.40 – 1.59) |
| Nordland |
5,213 |
93 |
71 |
95 |
135 |
132 |
1.86 (1.70 – 2.04) |
| Troms |
3,488 |
112 |
112 |
123 |
140 |
128 |
1.15 (1.03 – 1.28) |
| Finnmark |
1,391 |
112 |
91 |
94 |
119 |
116 |
1.28 (1.08 – 1.52) |
| [i] | |||||||
[i] 1 Gender and age distribution in Norway 1989 – 2008 as standard
² Rate ratio (RR) adjusted for gender and age, Poisson regression
³ Helse Sør and Helse Øst are considered as two separate health enterprises even after their merger on 1 June 2007.
Even though the differences between the regional health enterprises (fig 2) and the counties (tab 2) have decreased considerably over time, some variations remain. In the period 2006 – 08, the Helse Midt health region stood out, with 152 operations for every 100,000 inhabitants (tab 2). This represented a statistically significant higher frequency than in all other regional health enterprises, with the exception of Helse Sør. With regard to counties, there were still some major differences during the final period, even between counties within the same regional health enterprise (tab 2).
Discussion
The information on hip arthroplasties is based on data reported to the Norwegian Arthroplasty register. Data are reported directly by the surgeon, who usually fills in the form submitted to the register immediately after the operation. Even though this reporting of operations to the register is voluntary, we have reason to believe that the register is near-complete. Comparisons with information submitted to the Norwegian Patient Register (NPR) show that the number of primary hip arthroplasties reported to the Norwegian Arthroplasty Register constituted 97 % of the number of prosthetics reported to the patient register (21). This completeness of reporting has also been confirmed at the patient level in several hospitals (25) – (27). The validity of the reported information has also been investigated in one hospital and showed very satisfactory results with regard to the variables reviewed: side (left, right), type of operation (primary, revision) and the date of operation (25).
The fact that the patient’s reported place of residence was the current place of residence rather than the place of residence at the time of the operation could represent a weakness of the study design. However, in light of the age group in question, there is little reason to assume that many of the patients have moved to other counties or regional health enterprises (28).
The frequency of primary hip arthroplasties caused by idiopathic coxarthrosis has increased more than for the material as a whole. This could be due to improved access to surgery, but also to a change in indications for operation. It has been shown that if the operation is postponed and the patient’s condition deteriorates, then the outcome of the operation will be poorer (29, 30). This could probably to some extent explain why a higher number of operations than before are performed on young people with less assumed pain and better functional capability. Nevertheless, we found that the increase was most marked among the oldest patients. The increasing number of elderly people with good general health who are able to undergo hip arthroplasty, better anaesthetics and a general consensus of not using age as a contraindication for an operation, are factors that can explain this increase. It is crucial to investigate whether this change in indication for operation may change the results of hip arthroplasty surgery.
In recent years, we have seen that the frequency of primary hip arthroplasty has remained relatively constant, and one may ask whether existing surgical capacity is sufficient to cover demand for this type of surgery. A study published in 1999 showed that hip arthroplasty capacity in England fell six per cent short of demand (31). Comparable frequencies of primary hip arthroplasty have been reported for Norway and England (32), and if we assume that the prevalence of hip disorders that require implantation of a prosthesis also is similar, it is reasonable to claim that too few, rather than too many, are offered this type of surgery in Norway. Many studies estimate an increasing need for hip arthroplasty in the years to come, in light of an increasing proportion of elderly people in the population and also because an increasing number of young people (33) and elderly people undergo surgery (6, 33, 34). Further studies ought to be undertaken to clarify the need for future surgical capacity, with regard to Norway as well.
It has been shown that the frequency of primary total hip arthroplasties varies significantly in different countries (4). However, a study based on national registry data for the years 1996 – 2000 showed that the annual frequencies of arthroplasties caused by primary coxarthrosis were fairly similar in the Nordic countries (9). Differences could nevertheless be observed for groups of individuals. In concurrence with our study, Lohmann et al. (9) observed that the proportion with hip arthroplasty was twice as high among Norwegian women as among men, while this proportion was lower in the other Nordic countries, at 1.1 – 1.3.
Similar to the results of our study, considerable regional differences in the frequencies of primary total hip arthroplasties have been found in other countries as well (14) – (16). In a Danish study, differences related to diagnoses could not explain the regional variations (15). Investigating this issue in Norway is difficult, since generally little is known about the frequency of various diagnoses according to area of residence. Differences in the prevalence of coxarthrosis among various groups of the population have been demonstrated (35, 36), and it is conceivable that this can partly explain the low frequency of arthroplasty operations in some counties. For example, as of 1 January 2009, a total of 22 per cent of the population of Oslo had a non-Western background, compared to 8 per cent in the country as a whole (37). Another possible explanation includes the differences in attitudes to this type of operation among various groups of the population, reflected in surveys (38). For example, it has been shown that non-European patients have a higher level of discomfort before they undergo surgery, and that they assess this operation as dangerous to a higher extent than patients from a European ethnic background (39). Furthermore, studies have revealed a lower frequency of hip arthroplasty in large cities in countries such as England, Denmark, Sweden and Finland (14, 15, 17, 40). Attempted explanations refer to how the infrastructure and working conditions are better there than in rural areas, so that it is possible to cope without an artificial joint (14). A study from the US showed that low population density was correlated with a high frequency of hip arthroplasty (41), while other studies, on the other hand, show that regional differences cannot be explained by population density, or by factors such as density of orthopaedic surgeons, hospital costs and regional gross domestic product (14, 15, 17). In our study, we have not adjusted for factors such as differences in the extent of hospital coverage and surgical capacity, and further research should also investigate the effects of such factors in the Norwegian context. Geographical differences in the indication for an operation could also be a possible explanatory factor for the variations in frequency according to place of residence (14).
Tabell
| Main message |
|
- 1.
Garellick G, Malchau H, Herberts P et al. Life expectancy and cost utility after total hip replacement. Clin Orthop Relat Res 1998; nr. 346: 141 – 51. [PubMed]
- 10.
Graves SE, Davidson D, Ingerson L et al. The Australian Orthopaedic Association National Joint Replacement Registry. Med J Aust 2004; 180 (suppl 5): S31 – 4. [PubMed]
- 11.
Bourne RB, Maloney WJ, Wright JG. An AOA critical issue. The outcome of the outcomes movement. J Bone Joint Surg Am 2004; 86-A: 633 – 40. [PubMed]
- 12.
Hip and knee replacements in Canada. Canadian Joint Replacement Registry (CJRR) 2008 – 2009 Annual report. Ottawa: Canadian Institute for Health Information, 2009.
- 13.
Mahomed NN, Barrett JA, Katz JN et al. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am 2003; 85-A: 27 – 32. [PubMed]
- 14.
Mäkelä KT, Peltola M, Häkkinen U et al. Geographical variation in incidence of primary total hip arthroplasty: a population-based analysis of 34,642 replacements. Arch Orthop Trauma Surg 2010; 130: 633 – 9.
- 18.
Nasjonalt Register for Leddproteser. www.haukeland.no/nrl/ (6.7.2010).
- 20.
Furnes O, Havelin LI, Espehaug B et al. Det norske leddproteseregisteret – 15 nyttige år for pasientene og for helsevesenet. Tidsskr Nor Lægeforen 2003; 123: 1367–9. [PubMed]
- 22.
Statistisk sentralbyrå. www.ssb.no/ (6.7.2010).
- 23.
Woodward M. Epidemiology. Study design and data analysis. Boca Raton, FL: Chapman & Hall/CRC, 1999.
- 24.
National Cancer Institute. Standard populations (millions) for age-adjustment. http://seer.cancer.gov/stdpopulations/ (6.7.2010).
- 26.
Hulleberg G, Aamodt A, Espehaug B et al. A clinical and radiological 13-year follow-up study of 138 Charnley hip arthroplasties in patients 50 – 70 years old. Comparison of university hospital data and registry data. Acta Orthop 2008; nr. 5: 79.
- 27.
Frøen JF, Lund-Larsen F. Ti år med Lubinus Interplanta hofteproteser. Tidsskr Nor Lægeforen 1998; 118: 2767 – 71. [PubMed]
- 28.
Statistisk sentralbyrå. Flest flytter innenfor egen kommune. Samfunnsspeilet nr. 5/2005. www.ssb.no/samfunnsspeilet/utg/200505/05/index.html (6.7.2010).
- 29.
Espehaug B, Havelin LI, Engesaeter LB et al. Patient satisfaction and function after primary and revision total hip replacement. Clin Orthop Relat Res 1998; nr. 351: 135 – 48. [PubMed]
- 33.
Kurtz SM, Lau E, Ong K et al. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res 2009; 467: 2606 – 12.
- 37.
Statistisk sentralbyrå. Innvandrere og norskfødte med innvandrerforeldre, etter landbakgrunn. Fylke. 1 januar 2009. www.ssb.no/emner/02/01/10/innvbef/arkiv/tab-2009-04-30-09.html (6.7.2010).
- 39.
Gandhi R, Razak F, Davey JR et al. Ethnicity and patient’s perception of risk in joint replacement surgery. J Rheumatol 2008; 35: 1664 – 7. [PubMed]
- 41.
Peterson MG, Hollenberg JP, Szatrowski TP et al. Geographic variations in the rates of elective total hip and knee arthroplasties among Medicare beneficiaries in the United States. J Bone Joint Surg Am 1992; 74: 1530 – 9. [PubMed]