Main points
Manipulation techniques are used to counteract infant torticollis, but the use of such techniques is controversial
We performed a comprehensive literature review to identify and summarise research on the efficacy and safety of manipulation techniques
Research did not support the use of manipulation techniques in the treatment of infantile asymmetry, but there was uncertainty associated with the research findings
Torticollis is the collective term for asymmetries of the head and neck region. The prevalence of congenital muscular torticollis, which is often accompanied by asymmetric head shape, is estimated at about 1 % (1). A greater number of infants, around 10 % of all those under six months, have an asymmetric head shape that may be related to restricted range of motion of the neck and to a positional preference when supine (2). Figures from Statistics Norway and the Norwegian Health Economics Administration show that approximately 8 % of all Norwegian infants are taken to manual therapists in their first year, often due to head and neck-related asymmetries (3).
Conservative treatment of congenital muscular torticollis and other forms of asymmetry in infants, hereafter referred to as infantile asymmetry, consists of parental guidance, physiotherapy and home exercises (4, 5, 6). The aim is to establish symmetrical movement patterns through massage, passive stretching exercises and stimulation interventions (4, 7).
In the 1990s, H. Biedermann introduced the term cervical joint-induced symmetry disorder (also known as KISS, Kopfgelenk-induzierte Symmetrie-Störung), and described a possible association between imbalances of the cervical vertebrae in infants, symmetry disorders and symptoms such as colic and sleep and eating disorders (8, 9, 10). Biedermann believed that such imbalances could be treated with manipulation, i.e., brief gentle pressure applied with the index finger to the cervical joints (8). In Norway, this form of treatment is offered by practitioners in chiropractic, physiotherapy, manual therapy and osteopathy, but the efficacy and safety of manipulation techniques, especially in infants, is disputed (11, 12).
In this article, we searched for controlled studies that compared manipulation techniques with other treatments offered to infants with torticollis. We focused in particular on whether manipulation techniques contribute to more symmetrical posture and movement patterns, but we also considered the impact of treatment on autonomic outcomes like sleep, crying and restlessness. When searching for evidence of possible adverse effects, we considered all types of studies, irrespective of design.
Material and method
This article is an update of a systematic review published by the Norwegian Knowledge Centre for the Health Services in 2009 (13). A project plan was published in August 2015, describing the intended article in detail (14). In addition to using the search results from the earlier review (13), we also performed a search covering the period from the original search to August 2017. We conducted searches in MEDLINE, EMBASE, CINAHL, Cochrane CENTRAL, AMED, PEDro and the Index to Chiropractic Literature. The search was conducted by combining text and keywords describing the population (e.g. 'KISS', 'torticollis', 'asymmetric neck') and intervention (e.g. 'manual therapy', 'manipulation', 'osteopathy') (see appendix on tidsskriftet.no). We also searched for studies in the reference lists of other relevant reviews and studies.
To investigate efficacy, we included only controlled studies that fulfilled the selection criteria in Table 1. However, it can be difficult to detect rare adverse effects and harms in controlled studies. To investigate safety, we therefore allowed the inclusion of other types of studies too (Table 1).
Table 1
Criteria used to select studies to investigate the efficacy and safety of treatment. Studies that did not fulfil all criteria with respect to either efficacy or safety were excluded.
| Efficacy | Adverse effects | |
|---|---|---|
| Design | Randomised, quasi-randomised and non-randomised controlled studies | All, including case reports |
| Population | Infants (0–2 years) in whom cervical joint-induced symmetry disorder was suspected1 | Infants (0–2 years) treated for cervical joint-induced symmetry disorder1 |
| Intervention | Manual therapy, chiropractic, osteopathy and physiotherapy targeting the cervical spine | Manual therapy, chiropractic, osteopathy and physiotherapy targeting the cervical spine |
| Comparison | No treatment, or placebo or other forms of treatment not targeting the cervical joints | — |
| Outcome | Degree of symmetry, sleep disorders, duration of crying, passive rotation, etc. | Respiratory problems, nerve damage, paralysis, death, etc. |
1Studies on manipulation therapy for infants with colic were excluded.
Two of the authors selected articles independently of one another. Titles and abstracts were first reviewed for all hits from the literature search. Full-text articles were retrieved if at least one author considered the abstract to be relevant with respect to the selection criteria. An article was included if both authors agreed that it was relevant. Disagreements were resolved through discussion.
For studies that compared groups, we evaluated the risk of bias related to patient selection, study conduct, detection, follow-up and reporting using the Cochrane Collaboration's tool (15). This entails evaluation of factors such as randomisation procedures, masking, and dropout analysis. Studies without group-wise comparisons, which were included to reveal possible harms, were considered to have a high risk of bias. We contacted the Norwegian System of Patient Injury Compensation to obtain statistics on injuries reported after treatment of the neck by a chiropractor, manual therapist or physiotherapist.
Dichotomous outcomes were presented as relative risk (RR), and continuous outcomes as mean differences (MD) with 95 % confidence intervals. We used GRADE (Grading of Recommendations Assessment, Development and Evaluation) to assess whether we had high, medium, low or very low confidence that the reported outcomes resembled the true outcomes (16).
Results
The literature search resulted in the inclusion of six publications (Figure 1). Three of these were randomised controlled trials, two of which examined the efficacy of manual therapy (17, 18) and one, osteopathy (19). These studies are described in Table 2, which also summarises our rating of the risk of bias. In brief, the studies of Haugen et al. (17) and Philippi et al. (19) were exposed to few systematic sources of error. The study of Cabrera-Martos et al. (18) was considered to have methodological limitations that may have affected its conclusions. The limitations were primarily related to the lack of parental blinding, and to the fact that children in the manual therapy group received more frequent follow-up than those in the control group. These differences may have contributed to greater treatment compliance in the manual therapy group. Details of the therapeutic techniques are presented in Table 3.
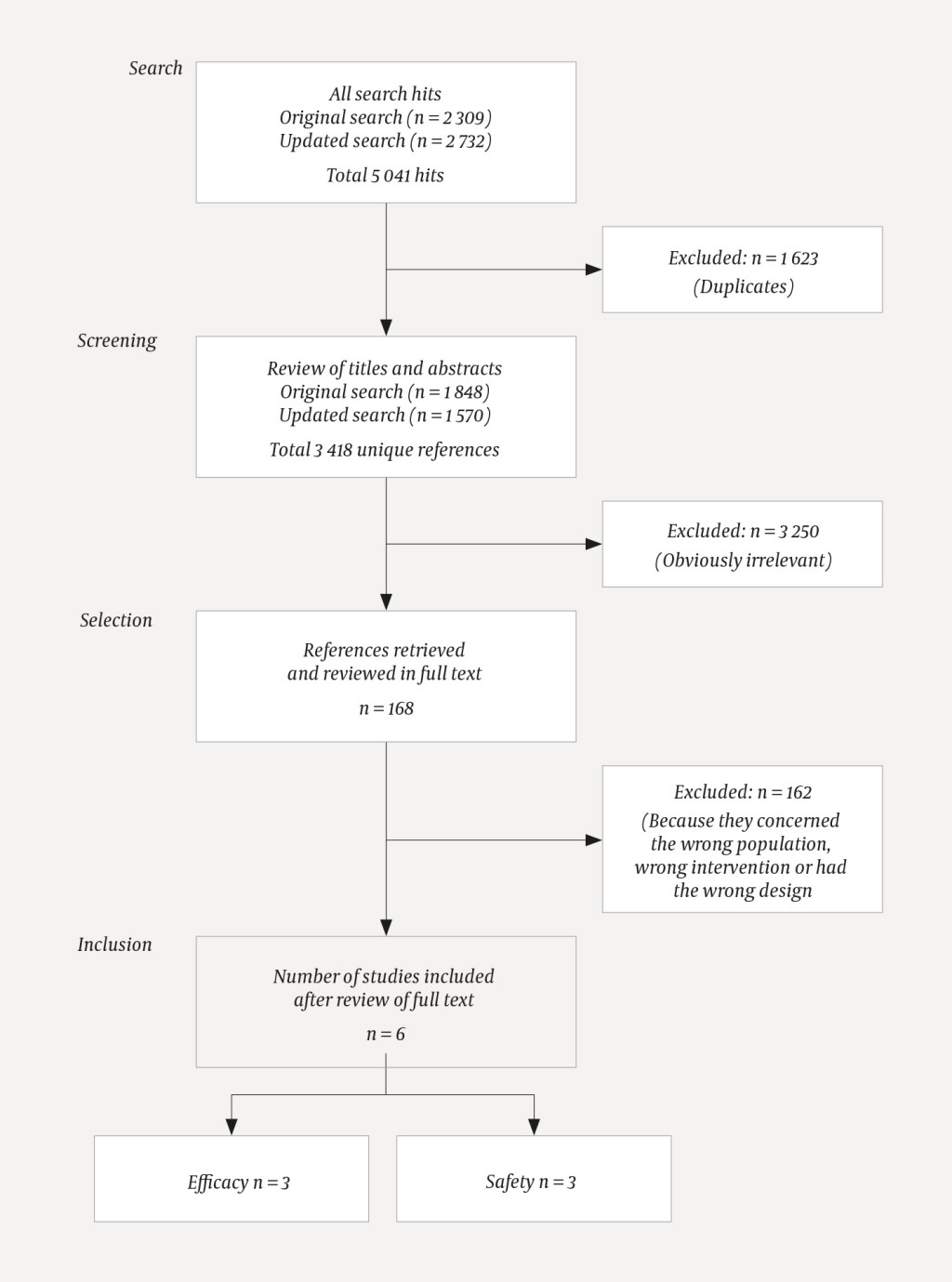
Table 2
Characteristics of studies used to examine the efficacy and safety of manipulation techniques for infantile asymmetry. The studies are arranged within each category according to year of publication.
| Study | Participants | Intervention | Control | Outcome | Risk of bias1 | GRADE assessment2 |
|---|---|---|---|---|---|---|
| Efficacy | ||||||
| Cabrera-Martos et al. 2016 (18), randomised controlled trial | 46 children with plagiocephaly, aged ~5.7 months | Standard + manual therapy, weekly 45-minute sessions | Standard: Orthotic helmet + parental advice | Motor development: | High | For both outcome measures: ⊕⊙⊙⊙ |
| Haugen et al. 2011 (17), randomised controlled trial | 32 children with reduced neck mobility, aged 3–6 months | Physiotherapy + manual therapy, two sessions of manual therapy | Physiotherapy alone | Change in symptoms5 after 8 weeks: | Low | ⊕⊕⊙⊙ |
| Philippi et al. 2006 (19), randomised controlled trial | 32 children with postural asymmetry, aged 6–12 weeks | Osteopathy, weekly treatment × 4 | Placebo | Asymmetry6: | Low | ⊕⊕⊙⊙ |
| Safety | ||||||
| Happle et al. 2009 (24), case report | 2 children with postural asymmetry, aged 6 and 15 months | Manual therapy + physiotherapy | — | Delayed diagnosis | High | — |
| Koch et al. 2002 (23), patient series | 695 children with postural asymmetry, aged 1–12 months | Chiropractic | — | Heart rate | High | — |
| Shafrir & Kaufman 1992 (25), case report | 1 child with postural asymmetry, aged 4 months | Chiropractic | — | Delayed diagnosis | High | — |
1Randomised controlled studies were assessed using the Cochrane Collaboration's tool (15), while a discretionary judgement was made that patient series and case reports were at high risk of bias
2Grading of Recommendations Assessment, Development and Evaluation (16)
3Precision (−2), estimated efficacy has a very wide 95 % CI owing to the small number of participants
4Risk of bias (−1) because of possible age difference between groups, lack of parental masking, and different frequency of follow-up
5Physiotherapist's assessment of torticollis symptoms based on video recordings: worse, no change, better or much better
6Scale – developed by the study authors – from 4 (full symmetry) to 24 (maximum asymmetry) points based on evaluation of video recordings
Table 3
Description of interventions used in the studies in this review.
| Study | Description of intervention | |
|---|---|---|
| Intervention group | Both groups | |
| Haugen et al. 2011 (17) | Two treatments by manual therapist. During treatment, the head was held in a central position without stretching any structures. The atlas was gently manipulated in a direction appropriate to the functional impairment of the joint. | Advice and follow-up from a paediatric physiotherapist with the aim of stimulating equal movement on both sides. The physiotherapists had broad scope in deciding what content to include in the follow-up, but they were not to stretch the neck against resistance from the child. |
| Cabrera-Martos et al. 2016 (18) | Weekly follow-up by manual therapist. The treatment was personalised, aimed to improve range of motion and function of the cervical spine, and predominantly targeted the spheno-occipital joint, atlanto-occipital joint and sacrum. | Advice on positioning and wearing an orthotic helmet 23 hours a day, plus monthly follow-up. |
| Philippi et al. 2006 (19) | Four treatments by an osteopath who was free to use any techniques deemed necessary to correct the disorder. Osteopathy may consist of massage, manipulation techniques and stretching. The first author has established, in personal communication, that the techniques used bear many similarities to manual therapy. | Advice on positioning. Children in the control group underwent the same tests as those in the intervention group, but without receiving active treatment. |
| Koch et al. 2002 (23) | One treatment by a chiropractor. During treatment, the infant was supine and all rotation of the spine was avoided. The therapist directed impulses (30 to 70 N) towards the suboccipital region on the side of the asymmetry. | — |
| Happle et al. 2009 (24) | Manual therapy and physiotherapy (details not specified). | — |
| Shafrir & Kaufman 1992 (25) | Chiropractic (details not specified). | — |
Manual therapy
Haugen et al. compared the efficacy of manual therapy as an adjunct to physiotherapy in infants aged between three and six months with reduced range of motion in the neck (17). The parents, the physiotherapists who performed the physiotherapy intervention and the individuals who evaluated the outcomes were unaware of which children had received manual therapy.
The children in the study were filmed at each visit. The recordings were used to quantify spontaneous motor function and strength as well as active and passive range of motion. The paediatric physiotherapist evaluated the final outcome by comparing recordings from the start of the study with those from the follow-up, and qualitatively assessing whether the child was worse, showed no significant change, was better or much better. After eight weeks, 12 of 15 participants in the treatment group and 13 of 16 in the control group were markedly better with fewer torticollis symptoms (RR 0.92, 95 % CI 0.16 to 5.49; see Table 2). There were no demonstrable differences between the groups in either symptom burden or in outcomes related to asymmetries in sleeping position, movement patterns, flexion or head rotation (17). Our confidence in the evidence is low for all outcomes owing to the small number of study participants and the imprecise effect estimates.
Cabrera-Martos et al. investigated the efficacy of manual therapy as an adjunct to parental guidance and treatment with an orthotic helmet (18). The children's motor development was assessed using the Alberta Infant Motor Scale (20), and asymmetry was classified according to the Argenta scale (21). At the end of the study, asymmetry was minimal (0 or 1) and motor development satisfactory for all 46 children who participated in the study (Table 2). The mean treatment duration in the control group was 149 days, which was 39 days longer (95 % CI 31–46) than for the children who received manual therapy. However, there is a high risk that the absence of parental blinding, and the fact that the children in the manual therapy group received more frequent follow-up than those in the control group, may have contributed to systematic biases.
Osteopathy
Philippi et al. randomised 32 infants with postural asymmetry to osteopathy or placebo (19). Children in the placebo group underwent the same tests as those in the intervention group but, for those in the placebo group, the osteopath placed his/her hands in the treatment position without performing active treatment.
The degree of symmetry was rated from 4 (full symmetry) to 24 (maximum asymmetry) using standardised video-based measurements (22). For participants in the control group, the symmetry score changed from 14.2 to 13.0, whereas for those in the osteopathy group, it changed from 15.4 to 9.5 (19). Children in the intervention group thus experienced an average improvement that was 4.7 points greater than in the control group (95 % CI 2.0 to 7.6 points; see Table 2). The authors did not provide effect estimates for the outcomes of vomiting, sleep, drinking, mood, excitability, defecation pattern and crying, but they found no statistically significant differences between the osteopathy and control groups (19). Due to the small number of study participants and imprecise effect estimates, we have low confidence in the evidence for all outcomes.
Risk of harm
The randomised studies included in this review did not report adverse effects, but we identified and included three descriptive studies – one patient series (23) and two case reports (24, 25) – to examine adverse effects and the risk of harm (Table 2).
Koch et al. presented data from 695 German infants who received manipulation treatment for cervical joint-induced symmetry disorders (23). No serious adverse effects were reported, but measurement of heart and respiratory rate revealed that manipulation treatment was often accompanied by transient apnoea and reduced heart rate, especially in the youngest children (23).
Happle et al. described two infants who were diagnosed with cervical joint-induced symmetry disorders and who were treated with manual therapy and physical therapy (24). Further investigation revealed that their symptoms, which persisted after completion of treatment, were due to cancer. The authors emphasised that infantile asymmetries may have serious differential diagnoses, and that delayed diagnosis can have serious consequences (24).
Shafrir & Kaufman described a four-month-old boy who was treated for infantile asymmetry by a chiropractor (25). After the manipulation, the boy quickly deteriorated. Examination revealed that the manipulation had triggered acute exacerbation of a previously undiagnosed intraspinal tumour (25).
Figures obtained from the Norwegian System of Patient Injury Compensation show that, since 2009, there have been no reports of injuries to Norwegian infants as a result of neck manipulations performed by chiropractors, manual therapists or physiotherapists. During the same period, 55 adult patients aged between 28 and 60 years sought compensation following neck manipulation by a chiropractor, manual therapist or physiotherapist. Eight had their claims upheld, including one in which the treatment was judged likely to have triggered a stroke.
Discussion
After reviewing the literature, we included three randomised controlled studies on the efficacy of manual therapy or osteopathy for infantile asymmetries of the head and neck. Haugen et al. showed that physiotherapy and manual therapy produced a change in symptoms similar to that seen with physiotherapy alone (17). Cabrera-Martos et al. suggested that manual therapy targeting the cervical spine may shorten treatment duration in infants with head asymmetries undergoing treatment with an orthotic helmet, but methodological limitations raise doubts about the result (18). Philippi et al. showed that a complex osteopathic intervention may potentially counteract asymmetry in infants with postural asymmetry, but found no differences between the osteopathy and placebo groups in defecation patterns, eating habits, sleep, mood and crying (19). We were unable to find any studies that examined the efficacy of chiropractic, or that investigated the risk of injury in a systematic manner.
Osteopathy and manual therapy have many common features, but there are key differences in the comparisons made by the efficacy studies in this review. Osteopathy was compared with placebo (19). Manual therapy was compared with conservative measures, but whereas Haugen et al. (17) designed their study to test the efficacy of manual therapeutic manipulation in isolation, Cabrera-Martos et al. (18) examined a more complex manual therapeutic approach. These differences mean that we were unable to combine the results in a meta-analysis, but the studies should nevertheless be considered in association with one another. One possible interpretation is that conventional physiotherapy and osteopathy both promote symmetrical development, but the specific manipulation or impulse technique used is not crucial to the end result.
The results we report in this article are consistent with other reviews on the topic (26–28), but some uncertainty remains over the conclusions. The small number of studies and participants means that there is uncertainty as to the true effect estimates. It could be argued that studies with alternative designs should also have been included. However, as infantile asymmetries often resolve spontaneously, uncontrolled studies would not provide reliable answers with respect to the issue of efficacy (29, 30).
There is anecdotal evidence that manipulation treatment has led to adverse events in adult patients (31). Adverse events have also been reported in children, but in the context of manipulation treatment performed on patients who had received an inadequate work-up (24, 25). Effective diagnosis and work-up are important to avoid delays in treatment and to prevent exacerbation of underlying disease (32, 33).
Irrespective of the risk of serious adverse events, it is important to consider whether treatment may cause the patient discomfort. In a survey of Norwegian manual therapists who treat infants, 25 % reported that children often begin to cry in association with treatment (3). It is ethically problematic to offer treatment of unproven efficacy to children, especially if the treatment entails discomfort (34). However, it is also important to be aware that not all infants taken to manual therapists, chiropractors or osteopaths due to asymmetries receive treatment with manipulation techniques (3). Half of Norwegian manual therapists report, for example, that they never manipulate the spine when treating infants, and that parental guidance is by far the most commonly used measure (3).
Data from Statistics Norway and the Norwegian Health Economics Administration show that approximately 8 % of all Norwegian infants are taken to manual therapists in their first year, often because of infantile asymmetry (3). This is in addition to treatments by chiropractors, osteopaths and other therapists. Why so many parents of infants seek help is unclear, but many may feel compelled to act if they perceive that their child differs from what is considered normal. A Finnish study showed that many concerns related to infantile asymmetries could probably be avoided if the parents receive good information and guidance when the child is born (35).
New parents are highly receptive to advice, and healthcare professionals should ensure that the advice given to parents, and the treatment given to children, is evidence-based and well-established. No causal relationship has been established between functional disorders of the neck and infantile asymmetries, and there is no reliable research to support the claim that untreated functional disorders of the neck give rise to complications and impairments later in life. This article, too, shows that the use of manipulation techniques to treat infantile asymmetries lacks evidence from research. Since the current evidence base consists of a small number of studies with few participants, it is difficult to draw firm conclusions, but our findings do not support the use of manipulation techniques in the treatment of infantile asymmetry.
- 1.
Cheng JC, Tang SP, Chen TM et al. The clinical presentation and outcome of treatment of congenital muscular torticollis in infants–a study of 1,086 cases. J Pediatr Surg 2000; 35: 1091–6. [PubMed][CrossRef]
- 2.
Boere-Boonekamp MM, van der Linden-Kuiper LT LT. Positional preference: prevalence in infants and follow-up after two years. Pediatrics 2001; 107: 339–43. [PubMed][CrossRef]
- 3.
Linge B. Kartlegging av undersøkelse og behandling som barnemanuellterapeuter i Norge benytter på spedbarn 0–12 måneder, – en survey. Mastergradsoppgave. Bergen: Universitetet i Bergen; 2014.
- 4.
Oleszek JL. Congenital torticollis. BMJ Best Practice. https://bestpractice.bmj.com/topics/en-gb/759 (17.8.2017)
- 5.
Van Vlimmeren LA, Van Der Graaf Y, Boere-Boonekamp MM et al. [Physical therapy reduces the risk of postural plagiocephaly in infants with a preferred supine position.]. Kinesitherapie 2011; 11: 9–10.
- 6.
van Wijk RM, Pelsma M, Groothuis-Oudshoorn CG et al. Response to pediatric physical therapy in infants with positional preference and skull deformation. Phys Ther 2014; 94: 1262–71. [PubMed][CrossRef]
- 7.
Kaplan SL, Coulter C, Fetters L. Physical therapy management of congenital muscular torticollis: an evidence-based clinical practice guideline: from the Section on Pediatrics of the American Physical Therapy Association. Pediatr Phys Ther 2013; 25: 348–94. [PubMed][CrossRef]
- 8.
Biedermann H. Kinematic imbalances due to suboccipital strain in newborns. J Manag Med 1992; 6: 151–6.
- 9.
Biedermann H. KIDD: KISS-induced dysgnosia and dyspraxia. How functional vertebrogenic disorders influence the sensorimotor development of children. In: Biedermann H, red. Manual therapy in children. Edinburgh: Churchill Livingstone, 2004: 303–12.
- 10.
Biedermann H. Manual therapy in children: proposals for an etiologic model. J Manipulative Physiol Ther 2005; 28: e1–15. [PubMed][CrossRef]
- 11.
Brand PL, Engelbert RH, Helders PJ et al. Systematic review of effects of manual therapy in infants with kinetic imbalance due to suboccipital strain (KISS) syndrome. J Manual Manip Ther 2005; 13: 209–14. [CrossRef]
- 12.
Sinding-Larsen C, Bjørnstad R, Grøgaard J. KISS–forklaringen på mange plager hos barn? Tidsskr Nor Legeforen 2011; 131: 338–9. [PubMed][CrossRef]
- 13.
Brurberg KG, Myrhaug HT, Reinar LM. Diagnostikk og behandling av spedbarn med mistanke om funksjonsforstyrrelser i øvre nakkeledd. Rapport. Oslo: Nasjonalt kunnskapssenter for helsetjenesten, 2009. https://brage.bibsys.no/xmlui/bitstream/handle/11250/2378092/NOKCrapport17_2009.pdf?sequence=1 (5.10.2018).
- 14.
Effekt av manuelle intervensjoner for behandling av spedbarn med nakkeleddsinduserte symmetri-forstyrrelser (KISS) – prosjektplan. Oslo: Nasjonalt kunnskapssenter for helsetjenesten; 2015.
- 15.
Higgins JPT, Altman DG, Sterne JAC. Assessing risk of bias in included studies. I: Higgins JPT, Altman DG, Sterne JAC, red. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. København: The Cochrane Collaboration, 2011.
- 16.
Balshem H, Helfand M, Schünemann HJ et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011; 64: 401–6. [PubMed][CrossRef]
- 17.
Haugen EB, Benth J, Nakstad B. Manual therapy in infantile torticollis: a randomized, controlled pilot study. Acta Paediatr 2011; 100: 687–90. [PubMed][CrossRef]
- 18.
Cabrera-Martos I, Valenza MC, Valenza-Demet G et al. Effects of manual therapy on treatment duration and motor development in infants with severe nonsynostotic plagiocephaly: a randomised controlled pilot study. Childs Nerv Syst 2016; 32: 2211–7. [PubMed][CrossRef]
- 19.
Philippi H, Faldum A, Schleupen A et al. Infantile postural asymmetry and osteopathic treatment: a randomized therapeutic trial. Dev Med Child Neurol 2006; 48: 5–9, discussion 4. [PubMed][CrossRef]
- 20.
Piper MC, Pinnell LE, Darrah J et al. Construction and validation of the Alberta Infant Motor Scale (AIMS). Can J Public Health 1992; 83 (suppl 2): S46–50. [PubMed]
- 21.
Argenta L, David L, Thompson J. Clinical classification of positional plagiocephaly. J Craniofac Surg 2004; 15: 368–72. [PubMed][CrossRef]
- 22.
Philippi H, Faldum A, Jung T et al. Patterns of postural asymmetry in infants: a standardized video-based analysis. Eur J Pediatr 2006; 165: 158–64. [PubMed][CrossRef]
- 23.
Koch LE, Koch H, Graumann-Brunt S et al. Heart rate changes in response to mild mechanical irritation of the high cervical spinal cord region in infants. Forensic Sci Int 2002; 128: 168–76. [PubMed][CrossRef]
- 24.
Happle C, Wetzke M, Hermann EJ et al. 'Cases against KiSS': a diagnostic algorithm for children with torticollis. Klin Padiatr 2009; 221: 430–5. [PubMed][CrossRef]
- 25.
Shafrir Y, Kaufman BA. Quadriplegia after chiropractic manipulation in an infant with congenital torticollis caused by a spinal cord astrocytoma. J Pediatr 1992; 120: 266–9. [PubMed][CrossRef]
- 26.
Dobson D, Lucassen PL, Miller JJ et al. Manipulative therapies for infantile colic. Cochrane Database Syst Rev 2012; 12: CD004796. [PubMed]
- 27.
Posadzki P, Ernst E. Is spinal manipulation effective for paediatric conditions? An overview of systematic reviews. Focus Altern Complement Ther 2012; 17: 22–6. [CrossRef]
- 28.
Posadzki P, Lee MS, Ernst E. Osteopathic manipulative treatment for pediatric conditions: a systematic review. Pediatrics 2013; 132: 140–52. [PubMed][CrossRef]
- 29.
Douglas NA, Browning M, Miller J. Chiropractic care for the cervical spine as a treatment for for plagiocephaly: A prospective cohort study. J Clin Chiropr Pediatr 2016; 15: 1274–9.
- 30.
Lessard S, Gagnon I, Trottier N. Exploring the impact of osteopathic treatment on cranial asymmetries associated with nonsynostotic plagiocephaly in infants. Complement Ther Clin Pract 2011; 17: 193–8. [PubMed][CrossRef]
- 31.
Ernst E. Manipulation of the cervical spine: a systematic review of case reports of serious adverse events, 1995-2001. Med J Aust 2002; 176: 376–80. [PubMed]
- 32.
Mordt AC. Hva kjennetegner spedbarn med KISS – En intertester-reliabilitet av manuellterapeutisk klassifisering. Mastergradsoppgave. Bergen: Universitetet i Bergen, 2009.
- 33.
Biedermann H. Differential diagnosis of KISS syndrome. Manuelle Medizin 1996; 34: 73–81.
- 34.
Markestad T. Leger og alternativ behandling. Tidsskr Nor Legeforen 2012; 132: 2409–10. [PubMed][CrossRef]
- 35.
Aarnivala H, Vuollo V, Harila V et al. Preventing deformational plagiocephaly through parent guidance: a randomized, controlled trial. Eur J Pediatr 2015; 174: 1197–208. [PubMed][CrossRef]
Konklusjon deres er: ”Siden dokumentasjonen er basert på et lite antall studier med få deltagere, er det vanskelig å trekke sikre konklusjoner, men våre funn understøtter ikke bruken av manipulasjonsteknikker i behandling av spedbarnsasymmetri”. Det synes ikke å være grunnlag for en slik generalisert konklusjon/anbefaling på basert på de tre studiene artikkelen gjennomgår.
Jeg, Elisabeth Skjetne, er fysioterapeut i hjem og barnehager i Bærum, med klinisk erfaring fra barn med asymmetri fra 0-6 år. Jeg henviser mange spedbarn med asymmetri til manuell terapeut. Det gjelder særlig babyer/barn med skjevhet i øvre nakkeledd og tilhørende dislokasjon i bekkenledd. Jeg opplever en raskere tilgang på en symmetrisk og koordinert motorikk når de får manuell terapi, noe som gir dem et nødvendig grunnlag for senere utvikling av motorikk, persepsjon og sosialt.
Det som er trist, er å møte barn, som har hatt vanlige helsekontroller, som henvises når de er 2-5 år gamle. Det typiske er at ingen forstår hva som er i veien. Ofte er barna oppvakte, men kan streve med uro, fysisk utagering, søvn, grov- og finmotorikk, påkledning, språk, tegning, lek med andre barn. De kan ha store ekstra ressurser i barnehagen og flere utredninger bak seg. Jeg har til enhver tid 5-6 av disse barna til oppfølging. De blir ofte oppdaget av barnehagen. De er mine favorittbarn: Det er god prognose når leddene er korrigert.
Jeg har noen enkle sjekkpunkter: Ansiktsvending i mageleie: Når barnet vender ansiktet den ene veien går bevegelsen lett, men anstrengt motsatt vei. Asymmetri i nakkehudfoldene er vanlig. Ved tilhørende dislokasjon i bekkenledd; barnet klarer ikke å hoppe med samlede ben. Det kan stå på det ene benet, men streve veldig på det andre. Sykling på tohjulssykkel er vanskelig; de bikker hodet og holder skjevt på styret. Inspeksjon av holdning viser skjevheter som har forplantet seg nedover. En 4-åring sa at det ble en "kræsj" når han så den ene veien, men ikke motsatt vei.
Jeg har samarbeidet med Barne- og ungdomspsykiater Ketil M.Klem som også gjør disse enkle undersøkelsene, og han finner stadig skolebarn med samme skjevheter i nakke og bekken. Disse barna får også manuell terapi med gode resultater. Men skjevutvikling som har stått lenge, har skapt spor som tar lang tid å rette opp.
Etter manuell terapi trengs muskulær opptrening av symmetri, balanse og koordinasjon. Noen ganger skjer en markant bedring, noen ganger tar det lengre tid. Barna trenger fortsatt spesialpedagogisk hjelp. De har hatt opplevd å ikke mestre på flere områder og har engstelse i forbindelse med dette. Rolleleken deres likner traumatiserte barns lek, og de har stort behov for å bli sett.
Det er da fortvilet med fagartikler som til tross for manglende forskning å vise til, er med på å vanskeliggjøre dette kliniske viktige arbeidet ved å gi foreldre og fagpersoner unødig skepsis.
Takk for kommentarer til artikkelen om manipulasjonsteknikker ved nakkeasymmetri hos spedbarn. Kommentarene gir oss mulighet til å dele flere refleksjoner og presiseringer. Artikkelen vi har publisert er en systematisk oversikt, det vil si at vi oppsummerer forskning om et avgrenset tema. Vi ønsket å finne svar på om manipulasjonsteknikker er et effektivt virkemiddel i behandlingen asymmetrier hos spedbarn. Vi fant at forskningen ikke gir et sikkert svar, men også at det lille som finnes av forskning ikke bygger opp under hypotesen om at spedbarn vil ha nytte av slik behandling. Konklusjonen i en systematisk oversikt skal være informert av tilgjengelig forskning, og konklusjonen gir dermed seg selv, men konklusjonen må selvfølgelig revurderes dersom det dukker opp ny forskning.
I sin kommentar uttrykker Skjetne og Motzfelt Klem bekymring for «fagartikler som til tross for manglende forskning å vise til, er med på å vanskeliggjøre dette kliniske viktige arbeidet ved å gi foreldre og fagpersoner unødig skepsis». Til det vil vi si at mangelen på forskning er høyst reelt, og at det er viktig at foreldre får informasjon om dette før de treffer beslutninger om behandling på vegne av sine barn. Sunn kunnskapsbasert praksis bør bygge på preferanser, forskning og erfaring. Alene kan erfaring og teorier være dårlige veivisere.